Introduction
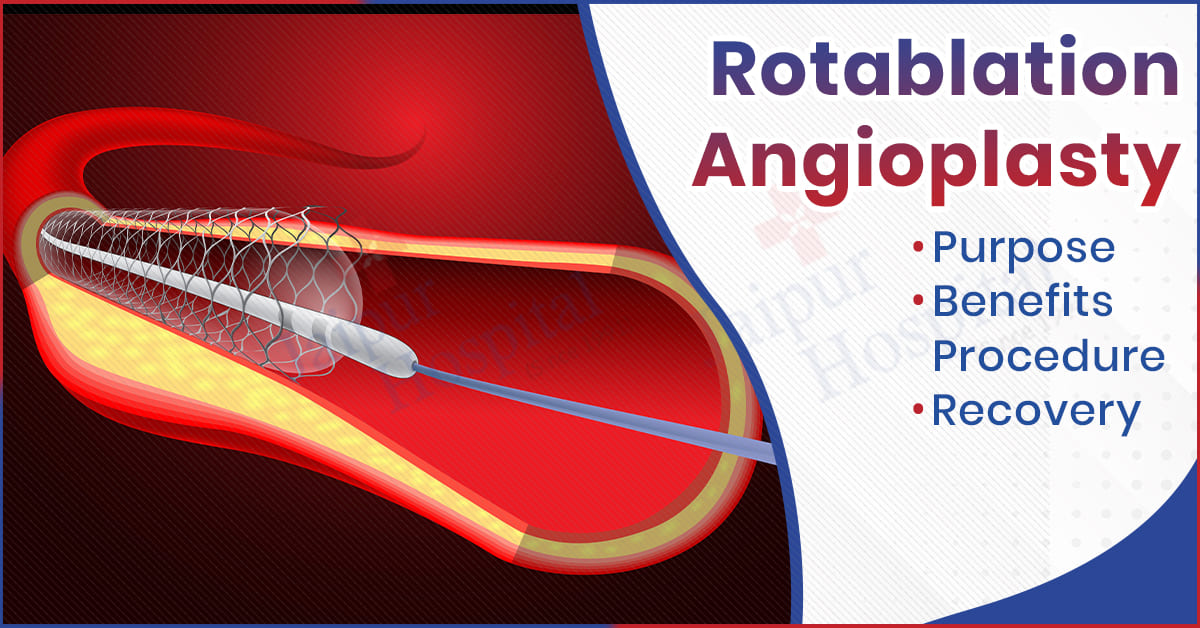
Rotablation angioplasty is a specialized-type treatment for tougher cases when the coronary arteries face extremely severe calcific blocks that cannot be treated by general angioplasty. The procedure uses a special device with a tiny burr rotating at high speeds to grind away the plaque, thereby easing the flow of blood to the heart.
The broader goal of this discussion is to examine the aims of rotablation angioplasty, its benefits, the procedure, the possible risks, and the expected days of recovery after treatment. We need to clarify the role of rotablation angioplasty treatment in the management of complex coronary artery disease in helping heart health.
What is Rotablation Angioplasty?
Rotablation Angioplasty: Rotablation angioplasty addresses a specific issue in the heart, namely closing off or narrowing of the coronary arteries due to calcified deposits. It is a tiny high-speed burr which has a diamond tip and a high speed. It gently and safely disperses the calcified plaque into the bloodstream. Blood flow is improved, and it is easier to put a stent in the rotablation angioplasty, making it a good treatment for patients whose blockages cannot be treated with normal angioplasty.
Why is Rotablation Angioplasty Needed?
Rotablation angioplasty is needed when conventional angioplasty cannot break through hard impenetrable blocks, especially in patients who have calcium deposits in coronary arteries or in advanced atherosclerosis involving vascular calcification. The main indications for open-heart operations are listed below:
- Severe Calcified Obstructions: When aorta or artery is severely impaired by calcium deposits in the root or the opening, either balloon angioplasty or a stent will not be placed.
- Standard Angioplasty Failure: It gets indicated if conventional angioplasty balloons fail to expand the narrowed artery effectively.
- Facilitation of Stent Placement: Rotablation improves the pace and expansion of stent by breaking down plaque.
- High-Risk Patients: It can be used for patients with multiple blockages, or those whose hearts are so bad, such that alternative treatments will not work.
- Restoring Blood Flow: This procedure helps to reestablish oxygenated blood to the heart muscles, reducing chest pains (angina) and averting other serious risks.
You Can Read Also: The Ultimate Guide to Boosting Immunity Naturally
Key Benefits of Rotablation Angioplasty
Traditional methods of treatment struggle the most with complex blockages, especially the calcified ones, and they require special procedures to provide the needed attention. For this type of treatment, the rotablation procedure provides the best solution with the following advantages in its angioplasty treatment:
- Proven Results in Difficult Cases: It is the only method that can successfully break up stubborn calcium buildups that other forms of angioplasty cannot.
- Improved Stent Placement: Reshaping the stiff plaque makes it easier to place stents and ensures they open properly, providing lasting benefits.
- Better Perfusion to the Heart: This procedure restores the perfusion of the heart when sufficient blood flow is brought back to perfuse the myocardium to diminish anginal pressure and alleviate dyspnea with exertion.
- Reduced Risk of Restenosis: Removal of plaque enhances stent results, helping to reduce arterial narrowing.
- Benefit to High-Risk Patients: Comes as an option for treating elderly patients or patients with multiple, high-risk blockages for whom usual interventions might not work.
- Relief of Symptoms and Improvement in Quality of Life: Patients generally report decreased frequency of anginal episodes, better tolerance for exercises, and feeling better, so that at the end they live a healthy and active life.
What is the Purpose of Rotablation Angioplasty?
Rotablation angioplasty targets patients with stiffened and calcified coronary artery occlusions that cannot be opened by regular angioplasty. The treatment provides the best preparation for the arteries for successful stent placement and sustaining improvement in the heart following treatment.
- Gradual Removal of Calcified Plaque: Achieving this objective helps eliminate the calcium deposits, which, otherwise, pose a challenge to the expansion of the angioplasty balloon.
- Supporting Stent Placement: Rotational atherectomy modifies the plaque, smooths the delivery path, and permits proper expansion inside the artery so the stent can be placed safely and effectively.
- Restoration of Blood Flow: After the surgery, blood would flow freely to the heart muscle to provide it with oxygen. This lessens the chances of the complications, including heart attack.
- Improving Patient Symptoms: Stabilization of chest pain, better breathing, and improved quality of life are factors for patients with coronary artery disease.
You Can Read Also: Brain Tumor: Symptoms, Causes & Treatments
What is the Procedure of Rotablation Angioplasty?
A rotablation angioplasty is a planned procedure performed by interventional cardiologists to deal with advanced, calcified blockages in the coronary arteries. Several steps are involved, each of which must be performed correctly for the procedure to be safe and effective. Therefore, the following provides a detailed account of the whole procedure:
- Preparation: Local anesthesia and light sedation are used to prepare the patient for the procedure, and a catheter is placed in an artery, most often through the wrist or groin.
- All the coronary arteries must at the least be punctured by the guiding catheter for blockage to be accessed.
- Rotablation device is introduced: The wire is successfully passed over the obstruction, at which time the rotablation device with its diamond-tipped burr is passed.
- Altering plaque: Restricting the diamond burr to ultrahigh velocity, the calcific deposits are gently abraded away, first into small particles, which are harmless and eliminated into systemic circulation.
- Balloon angioplasty and stenting: Once plaque modification has taken place, the artery is further expanded with a balloon, and a stent is placed to keep the artery open.
- Completion: The devices are removed, and the patient is assessed for stability before moving on to recovery.
How long does Rotablation Angioplasty take to recover?
The recovery time will depend on the patient’s health, severity of blockages, and whether the procedure was successful. Recovery time is still faster than full open-heart surgeries anyway, but the hospital stay is longer because of the medical requirements. Here are a few important things to consider:
- Hospital Stay: After the rotablation angioplasty procedure, the majority of patients remain in the hospital for 1 to 2 days for stabilization and heart function monitoring.
- Early recovery: Usually, a few days of home rest are suggested and no taxing activities for at least a week.
- Back to Normal Life: People may return to work and normal activities (such as going out in public and eating plenty of seating and walking) can return in 1–2 weeks or so on the advice of a doctor.
- Treatment and Lifestyle Modifications: Medications and heart-healthy lifestyle is the treatment and it includes quitting smoking and follow-up appointments.
- Long-Term Recovery: Patients enjoy considerable relief from symptoms such as chest pain and breathlessness, leading to an improved quality of life, assuming appropriate care is taken.
Conclusion
Summarizing, rotablation angioplasty is a specialized cardiac treatment used to address challenging, heavily calcified obstructions. It operates by cleaning out the hard blockage so that a stent can be inserted, to allow proper blood flow to resume. Although rotablation angioplasty does pose some risk, its benefits generally outweigh those risks, and are particularly appropriate for high-risk patients.
This is the Cardiology Department´s zone, and Jaipur Hospital is renowned for its rotablation for the angioplasty procedure. They have the cutting-edge machinery and expert cardiologists to treat the patient and oversee their recovery.